Neuropsychology Of Dysthymia: Anatomy Of Chronic Sadness
Persistent depressive disorder does not always respond to the pharmacological approach. This chronic apathy, hopelessness and bad mood have a more complex origin than we might think. The neuropsychology of dysthymia therefore reminds us that this condition is linked to a series of brain processes and social situations to be taken into account.
There is one detail that we cannot ignore when looking at the incidence of dysthymia in the population. Clinical studies indicate that this disorder affects 5% of the population, especially women. However, specialists know that many people live with a psychopathological framework without taking the plunge, without asking for help. This helplessness and rejection is chronified in such a way that the probability that the incidence data is greater than what we think is great.
It should also be noted that many studies have been carried out since the term “dysthymia” was replaced by “persistent depressive disorder” in the last volume of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) , with only one goal. The medical and scientific community seeks to better define and understand this condition. We are faced with much milder illness than major depression. However, given the difficulty in treating this condition, it is common for many patients to end up drifting at some point to other mental conditions and disorders.
Neuropsychology of dysthymia (persistent depressive disorder)
It was the psychiatrist Robert Spitzer who, in the 1960s, defined and “purified” this clinical condition, differentiating it from other poorly adapted terms. Until this famous specialist worked to improve and polish the classification of mental illnesses, dysthymia was more associated with a personality type. It defined people with a depressive, neurotic and low mood approach.
Persistent depressive disorder has continued to be refined since that time in order to get to the root of the problem. So the following qualifying conditions must be met for a person to receive this diagnosis:
- Depressed mood with a minimum duration of 2 years
- Presence of at least two of the following characteristics
- Loss or increased appetite
- Insomnia or hypersomnia.
- Lack of energy or fatigue
- Low self-esteem
- Concentration deficits or difficulty making decisions
- Feelings of hopelessness
- Ill-being, continuous suffering
- No psychotic, manic, other organic illnesses or suspected major depression
What happens to my brain if I am diagnosed with recurrent depressive disorder (dysthymia)?
A person often feels relief when they are diagnosed. The reason is obvious. Some have been dragging this shadow since adolescence. This emptiness that constantly entered through a door ajar to release discouragement and that lingering smell of sadness that envelops everything.
The neuropsychology of dysthymia tells us that this condition has an origin. We believe that stress and this increase in catecholamines and hormones such as cortisol affect our ability to regulate mood.
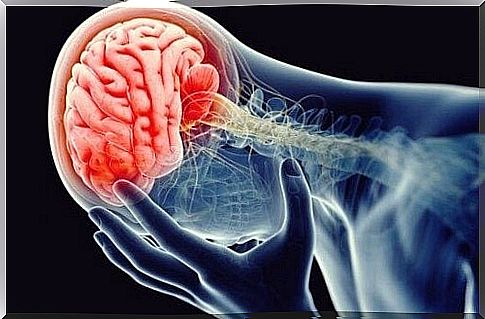
- Clinical research, including advances in the technology of brain imaging, such as magnetic resonance, we have offered the possibility to obtain very revealing data. One of them is the presence of low activity in all areas of the brain related to problem solving, sleep regulation, appetite and even our sociability.
- Most of these processes are concentrated in a very special area. This is the anterior cingulate cortex, responsible for executive and emotional control, which shows low activity in all patients with recurrent depressive disorder.
The cingulate cortex and Von Economo neurons
- The anterior cingulate cortex is part of a network responsible for generating several processes. It helps us process information, both sensory and emotional. It helps us maintain our attention while we are moving or interacting with others. It is this which facilitates the maintenance of interest in our environment. Which acts as a bridge between emotion and attention.
- This region of the brain also contains the Von Economo neurons. We have all heard of mirror neurons. Von Economo neurons also deserve our attention for one essential reason. These nerve cells connect with others to facilitate and process information relating to pain, hunger. They are also the ones that stimulate the generation of “social emotions” such as trust, love, resentment…
- Von Economo neurons are also found in monkeys, dolphins, whales and elephants. Animals that, like us, are depressed, also testify to the so-called “social suffering”. In other words, factors such as loneliness, rejection or loss of a position in the hierarchy of their group can generate sadness and emotional pain for them.
So these are very interesting data.

In conclusion: in search of answers
At this point and knowing what the neuropsychology of dysthymia tells us, the question is : what causes these areas related to this disorder to stop functioning as they should? More so, what can we do to make them regularize again? It is necessary to continue to study these questions in depth since these states are prolonged in time and do not always react to the pharmacological approach.
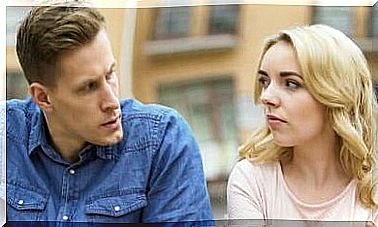
We know, for example, that there is a hereditary component. Likewise, the feeling of isolation or of having suffered a loss, or the simple fact of not feeling useful at a given moment generates these chronic states of suffering. The neuropsychology of dysthymia tells us that many patients often improve their condition when they start new projects. Just making a change in our life and feeling involved again in something or with someone generates such a positive step forward as we hoped for.
Don’t give up. We will be able to provide better answers as we learn more about these diseases. We know this at the moment: dysthymia is treatable. A good intervention and a psychotherapeutic approach make it possible to overcome it.